The Canadian Managed Alcohol Program Studies (CMAPS)
CISUR has led several studies of Managed Alcohol Programs in Canada. The initial Canadian Managed Alcohol Program Study (CMAPS) project, launched in 2013, rigourously evaluated MAPs in Canada and generated insights into their implementation and effectiveness. The results of this research will be used to reduce unintended negative consequences of MAPs and inform the development of program and policy recommendations.
Read about CMAPS findings published in Drug and Alcohol Review.
The CMAPS team is now pilotting and evaluating a cannabis substitution intervention as a component of MAPs for people with severe alcohol use disorders experiencing unstable housing. Read more about this project.
see more: An Overview of MAPs in Canada.
Featured resources
- Canadian Operational Guidance: Managed Alcohol Programs
- Operational Guidance for Implementation of Managed Alcohol for Vulnerable Populations
- Cannabis and alcohol harm reduction
- Safer Drinking Tips During COVID-19
- Scaling up of Managed Alcohol Programs guide
Overview of MAPs in Canada
Journal Articles/Research Papers
CMAPS research:
- Evaluating cannabis substitution for alcohol within the context of a canadian managed alcohol program (International Journal of Drug Policy, 2025)
- Access to healthcare among managed alcohol program participants: A mixed methods study (International Journal of Drug Policy, 2025)
- “Give me the reigns of taking care of myself with a home”: Healing environments in an Indigenous-led alcohol harm reduction program (Harm Reduction Journal, 2024)
- Participation in Canadian Managed Alcohol Programs and Associated Probabilities of Emergency Room Presentation, Hospitalization and Death: A Retrospective Cohort Study (Alcohol and Alcoholism, 2022)
- "If I knew I could get that every hour instead of alcohol, I would take the cannabis”: need and feasibility of cannabis substitution implementation in Canadian managed alcohol programs (Harm Reduction Journal, 2021)
- Trajectories of Alcohol Use and Related Harms for Managed Alcohol Program Participants over 12 Months Compared with Local Controls: A Quasi-Experimental Study (Alcohol and Alcoholism, 2021)
- Breaking the cycle of survival drinking: insights from a non-residential, peer-initiated and peer-run managed alcohol program (Drugs: Education, Prevention and Policy, 2020)
- “There is a Place”: impacts of managed alcohol programs for people experiencing severe alcohol dependence and homelessness (Harm Reduction Journal, 2019)
- Managed alcohol programs in the context of Housing First (Housing, Care and Support, 2019)
- Clients Perspectives of Managed Alcohol Programs in the First Six Months and Their Relational Shifts (MA Thesis, 2019)
- On the outside looking in: Finding a place for managed alcohol programs in the harm reduction movement (2019)
- Community managed alcohol programs in Canada: Overview of key dimensions and implementation (2018)
- Managed alcohol programs: Is it time for a more radical approach to reduce harms for people experiencing homelessness and alcohol use disorders? (2018)
- How do people with homelessness and alcohol dependence cope when alcohol is unaffordable? A comparison of residents of Canadian managed alcohol programs and locally recruited controls. Drug and Alcohol Review (2018)
- Counting the cold ones: A comparison of methods measuring total alcohol consumption of managed alcohol program participants. Drug and Alcohol Review (2017)
- Does managing the consumption of people with severe alcohol dependence reduce harm? A comparison of participants in six Canadian managed alcohol programs with locally recruited controls. Drug and Alcohol Review (2017)
- Finding safety: A pilot study of managed alcohol participants’ perceptions of housing and quality of life. Harm Reduction Journal (2016).
- Do managed alcohol programs change patterns of alcohol consumption and reduce related harm? A pilot study. Harm Reduction Journal (2016).
Other MAPs research:
- Exploring Nurses’ Perceptions of a Managed Alcohol Program at an Acute Care Hospital. The Canadian Journal of Addiction (2019).
- Research into action? The Eastside Illicit Drinkers Group for Education's (EIDGE) experiences as a community-based group in Vancouver, Canada (Commentary). Drug and Alcohol Review (2017).
- Shelter-based managed alcohol administration to chronically homeless people addicted to alcohol. CMAJ (2006).
Reports/guidance
CMAPS research:
- Canadian Operational Guidance: Managed Alcohol Programs (2023)
- Cannabis and alcohol harm reduction
- Safer Drinking Tips During COVID-19 (2020)
- Operational Guidance for Implementation of Managed Alcohol for Vulnerable Populations (2020)
- CISUR Bulletin 20: Scale up of Managed Alcohol Programs (2020)
- tawāw pe-apik | poohsapoot, amo ihtopiit | edanigha, hoɁa | annaii t'sat dhiindii ts'at nizheh da'on tinich'uh | qain, aimaruatun aquviatin | come and sit and be at home: A report based on sharing circles with residents and staff from Ambrose Place (2018)
- Towards alcohol harm reduction: Results from an evaluation of a Canadian Managed Alcohol Program in Sudbury, Ontario (Executive Summary) (2018)
- A Community Symposium on Mobilizing Local Responses in Victoria, BC (2018)
- A cost-benefit analysis of a Canadian Managed Alcohol Program: A report prepared by the Centre for Addictions Research of British Columbia for the Kwae Kii Win Centre Managed Alcohol Program (2016)
- CARBC Bulletin #9: Evaluation of a managed alcohol program in Vancouver, BC: Early findings and reflections on alcohol harm reduction (2013)
Other MAPs research:
- Outil d’orientation pour les milieux d’isolement COVID-19 accueillant des personnes en situation d’itinérance ayant une consommation d’alcool régulière et prolongée (Orientation tool for COVID-19 isolation settings for homeless people with regular and prolonged alcohol consumption) (2021) by Institut universitaire sur les dépendances, Direction de l'enseignement universitaire et de la recherche, CIUSSS du Centre-Sud-de-l'Île-de-Montréal
- Identifying the Integrated Harm Reduction Housing and Care Needs of Urban Indigenous Older Adults (2020) from the University of Calgary
- HR HOPEH - Harm Reduction Housing for Older People with Experiences of Homelessness (2020) from the University of Calgary
- Managed Alcohol Supports Toolkit: Community of Learning Report (2020) from the University of Calgary
- Harm reduction interventions for chronic and severe alcohol use among populations experiencing homelessness: A literature review (2018) from the University of Regina
- A Selective Literature Review on Managed Alcohol Programs and Indigenous Healing Methodologies (2017) from the Aboriginal Standing Committee on Housing and Homelessness, Calgary, Canada
-
Managed Alcohol Programs in Manitoba: Feasibility Report (2018) prepared by Sunshine House in Winnipeg, Canada
Evaluation materials
Infographics/posters
|
CISUR/EIDGE Poster: Safer Drinking Tips (pdf, 2018) |
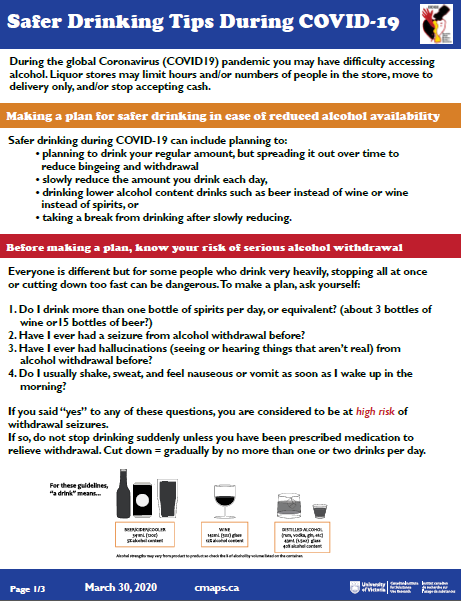
CISUR/EIDGE Poster: Safer Drinking During COVID-19 (pdf, 2020) |
 |
|
|
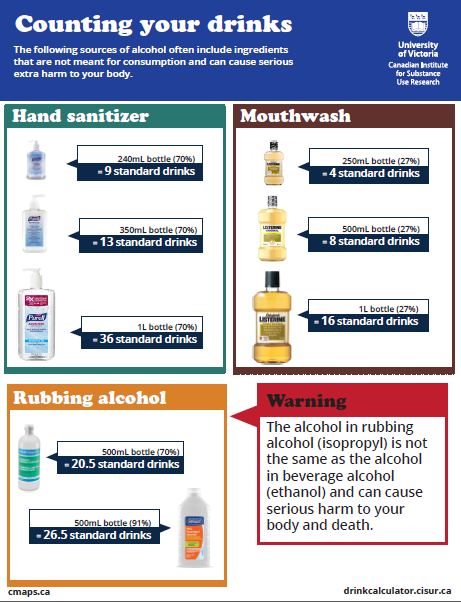
CISUR Poster: Counting your Drinks (pdf, 2018) |
CISUR Poster: Counting your Drinks (including non-beverage alcohol) (pdf, 2018) |
|
|
|
|
CISUR Infographic: Insights From a Peer-led Managed Alcohol Program (pdf; 2020) |
CISUR Infographic: Substituting cannabis in a Managed Alcohol Program: Could it work? (2021) |
 |
|
|
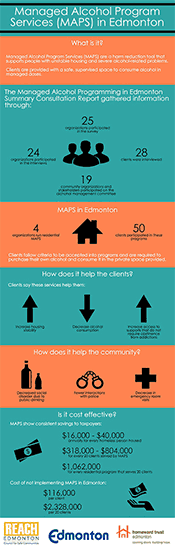
REACH Edmonton Infographic: MAPs in Edmonton (pdf) |
CISUR Infographic: Inside a Managed Alcohol Program in Thunder Bay, Ontario (pdf; 2016) |
 |
PowerPoint Presentations and Other Tools
- Learnings (and stories) from the Canadian Managed Alcohol Program Study (CMAPS)-Issues of Substance Conference, November 27, 2019, Ottawa, Ontario
- Evaluating Effectiveness of Alcohol Harm Reduction and Housing Instability
- Towards alcohol harm reduction and housing stability: Preliminary findings of Thunder Bay managed alcohol programs (email to request a copy)
Standard Drink Calculator
Webinars + E-newsletters
View/subscribe to the CMAPS e-newsletter
"Community of Practice" (CoP) Webinars:
Videos
- Video: The Pour: Treating Alcoholics with Wine (CBC Fifth Estate | Jan 2017)
- and The Pour: Update (CBC Fifth Estate | Dec 2017)
- Video: Do Managed Alcohol Programs Prevent Harms for People with Alcohol Dependence? - CISUR's Bernie Pauly & Tim Stockwell public talk (Sept 2016)
- Video: Introducing the Harm Reduction Program of CMHA-Sudbury/Manitoulin
- Video: Ottawa's managed alcohol program
- Video: The value of harm reduction (Thunder Bay)
- Video: Managed alcohol program (Vancouver)
- Video: Ryan Arcand, Edmonton's piano man (Edmonton)
Related News Stories
About MAPs and this project
MAPs originated as a response to the complex needs of people who do not respond to abstinence programs and are experiencing homelessness or housing instability . MAPs offer regulated access to beverage alcohol, alongside meals, healthcare, accommodation, and a range of social supports.
In Toronto, a managed alcohol program (MAP) was initiated in the late 1990’s following a coronial enquiry into the freezing deaths of problem drinkers who had been denied access to shelter accommodation. Emulated in other sites in Canada, MAPs involve the provision of accommodation, alongside controlled access to alcohol to replace non-beverage alcohol and reduce heavy drinking episodes for individuals who have often been unsuccessful in abstinence based treatment.
This harm reduction approach is a response to the harms of unstable housing and severe alcohol problems that have not been responsive to abstinence-based treatment. Related motivation is to encourage reduced use of non-beverage sources of alcohol such as methylated spirits, rubbing alcohol, hand sanitizer and mouthwash.
We conducted a national mixed methods study to investigate the implementation and outcomes of MAPs in Canada. Benefits, potential harms and best practices were investigated by accessing health and police records, conducting brief interviews monthly for up to two years and in-depth interviews with clients and program staff.
Findings to date
Findings from our initial evaluation of the Managed Alcohol Program (MAP) in Thunder Bay indicated that the objectives of the program to reduce harm and improve quality of life for MAP program participants were being met. This success was evidenced by the overall pattern of improvement in formal indicators related to housing, mental and physical well-being, reductions in alcohol-related harms, decreasing non-beverage alcohol (NBA) use and more stable patterns of alcohol consumption. Further, the observed substantial reductions in hospital admissions and times in police custody indicate substantial economic savings for the local community. The MAP participants reported reductions in rates of police contacts, hospital admissions and detoxification admissions of between 40% and 80%. There was also a reduction of NBA use and, although some use did continue, it was at a lower level.
An overarching achievement of the program was the creation of a safe and stable environment reported by participants in both qualitative and quantitative data. This was striking and stands in sharp contrast to the harms this population is exposed to on the street. The safety and stability provided by the program also enabled many participants to reconnect with family members and have greater feelings of self-worth and well-being.
Data collection is complete and occurred in two phases. Phase I included six sites with 175 MAP participants and 189 controls recruited. Eighty MAP participants and staff across sites completed qualitative interviews. During Phase II, we expanded data collection and conducted additional analysis allowing for a larger sample, longer term follow up of participants and controls. We secured health records to allow for long term analysis of morbidity and mortality of 205 MAP participants and 128 controls.
Our research has contributed significantly to a previously nascent body of knowledge. Our initial pilot studies of MAPs found evidence of reductions in some alcohol related harms, improved quality of life and safety, more stable housing and fewer demands on the health and criminal justice systems for MAP participants and reduced costs. Management issues related to eligibility criteria and tailoring programs to individual needs were identified as important to reduce harms. Our Thunder Bay pilot study was the first to include a control group and was a model for our current national MAP research. In an analysis of baseline data from 367 people with severe AUDs and unstable housing from six Canadian cities, MAP participants consumed alcohol on more days per month but overall consumed less alcohol per day and experienced fewer acute and social harms than controls. As well, MAP participants tended to use fewer negative coping strategies when alcohol was unaffordable than did controls. Qualitatively, participant identified that MAPs provided a safer space that allowed opportunities for healing and recovery.
Publications of both qualitative and quantitative findings can be foundin the publications section of this site, along with multiple presentations and research bulletins and an overview of programs in Canada. The MAP Community of Practice is well established with over 300 members and includes an active list serv as well as virtual events. Webinars and teleconferences alternating each month to share learnings and best practices as well as exchange of research findings and ideas. The Canadian Managed Alcohol Program Study is collaborating internationally with partners examining feasibility, development and evaluation of MAPs in Scotland and Australia. Provincially, we developed operational guidance for MAPS during COVID and a research bulletin on the scale up of MAPs as well as safer drinking guidelines. We are undertaking research related to implementation and evaluation of MAP during COVID across BC. In Canada, we are collaborating on Indigenous led research on alcohol harm reduction to design, develop and evaluate an Indigenous led and informed managed alcohol program.
Funding bodies
What is a MAP?
A managed alcohol program (MAP) is a harm reduction approach aimed at preventing some of the harms of severe alcohol dependence, often for people experiencing chronic homelessness or housing instability.
In a MAP, tailored amounts of beverage alcohol are provided to participants as a means to reduce harms related to alcohol use and replace non-beverage alcohol use. These small doses of alcohol are usually dispensed to the participant at regular intervals throughout the day. By providing smaller doses of beverage alcohol MAPs participants have the opportunity to safely stabilize or reduce their alcohol consumption as well as to replace non-beverage alcohol (e.g., mouthwash, hand-sanitizer, hairspray) with less harmful beverage alcohol.
In Canada, most MAPs are incorporated into residential programs like shelters, supportive housing and long term or residential care. In recent years MAPs have opened in non-residential settings like drop-in centres and hospitals.
How did MAPs in Canada get started?
What are the objectives of a MAP?
MAPs were created to help reduce harms related to alcohol dependency. MAP participants are people who experience severe alcohol dependency and in many cases have failed at other methods of alcohol treatment. There are three categories of harm associated with alcohol dependency that MAPs aim to reduce:
- “acute” comprising injuries, poisonings, or acute illnesses caused in part by heavy alcohol consumption;
- “chronic” comprising a range of serious illnesses including liver disease, cancers, strokes, and gastrointestinal diseases which are caused by the overall volume of alcohol consumed over time; and
- “social” comprising problems relating to housing, relationships, employment, finances, and crime (Rehm et al., 2001, p. 1418).
Many MAP participants have experienced a range of harms related to alcohol use and alcohol withdrawal. These harms are compounded when the majority of drinking is occurring in potentially dangerous street-based settings.
What is alcohol harm reduction?
Alcohol harm reduction recognizes that abstinence is not achievable or appropriate for everyone and helps address the acute, chronic and social harms associated with drinking alcohol.
MAPs are designed with an overarching alcohol harm reduction approach to health care and service delivery.
There are a variety of models that inform the design and implementation of MAPs. Many programs are based within Housing First models that employ both housing and alcohol management as primary interventions to reduce alcohol-related harm. Some programs are led by people with current or lived experience of street drinking (peers). Other programs are led by Indigenous organizations and perspectives, or work in partnership with Indigenous organizations to provide opportunities for participants to connect with cultural practices and ceremony.
Are there different types of MAPs?
Currently there are over 15 known MAPs across Canada. Each program is unique and created to address the needs of their specific communities. All 15 MAPs can be categorized as residential, non-residential or hospital-based. MAPs help stabilize a person’s alcohol consumption so they can focus on other areas of their health and well-being.
- Residential MAPs are programs that have a shelter or housing component that is connected to the MAP. Most Canadian MAPs are incorporated into residential programs like shelters, supportive housing and residential care.
- Non-residential MAPs are stand-alone programs. These programs are not associated with a specific housing program and only operate during the day. Non-residential MAPs are connected to other services and often help members access housing and social service supports.
- Hospital-based MAPs are established in conjunction with medical professionals who recognize that, in some cases, providing alcohol to patients while in hospital could help facilitate their care. Hospital-based MAPs are able to offer MAP support to those who may also require more intensive medical care. Detoxing from alcohol while in hospital can be dangerous. If a patient is already enrolled in an existing MAP or will resume alcohol use as soon as they are discharged, it might not be beneficial overall if they must cease alcohol use during their hospital stay. Participants in hospital-based MAPs are individually assessed to see if these services are suitable for their care plan.
In some cases, hospital-based MAP supports may be delivered directly through a specific “in-hospital” MAP and in others non-hospital-based residential and non-residential MAPs may be able to provide MAP supports on a temporary basis for participants while in hospital.
Please view our MAP registry for more details on each of the MAPs.
What populations do MAPs serve?
MAP participants are people who experience severe alcohol dependency and in many cases years of chronic homelessness or housing instability. Many MAP participants have tried and failed at other methods of alcohol treatment or have not been responsive to abstinence-based treatment (e.g. detox, rehab, AA). Alcohol dependency can be a serious condition that in some cases can be fatal. These risks are compounded when the majority of drinking is occurring in potentially dangerous street-based settings.
Do MAPs provide alcohol to participants?
Yes, MAPs dispense alcohol to participants. The numbers of drinks delivered in a MAP is based on the individual needs and goals of each MAP participant. For example, some participants may get one standard drink hourly and others maybe get one and a half standard drinks every ninety minutes. Some participants may also start their dosing earlier in the morning depending on the severity of their alcohol withdrawal symptoms. In some cases participants may request that their number of doses be reduced or watered down with juice for a period of time. Overall, most MAPs offer up to between 12-15 standard drinks of alcohol per day (Ramsperger & Ramage, 2017) dispensed by program staff. Prior to receiving each dose of alcohol, MAP participants are typically assessed by staff to avoid over-intoxication. Most MAPs provide beer or wine, although participants may contribute to alcohol costs through a program fee or bring in their own alcohol to be dispensed through the program.
What is CMAPS?
The Canadian Managed Alcohol Program Study (CMAPS) is a research project funded by the Canadian Institutes for Health Research (CIHR) Partnerships for Health System Improvement grant. CMAPS Phase I ran from May 2013 to June 2016 and Phase II began in July of 2016 and will continue until March 2019. Additional funding for CMAPS has been provided by the Michael Smith Foundation for Health Research, Vancouver Coastal Health and the Centre for Addiction and Mental Health.
In phase I, CMAPS aimed to provide a rigorous evaluation of health and social outcomes for 200+ program participants across five Canadian MAP sites in comparison with 200+ similar individuals recruited from nearby non-MAP agencies. Benefits, potential harms and best practices will be investigated by accessing health and police records, conducting brief interviews monthly for up to two years and in-depth interviews with clients and program staff. The results from phase I are currently being analyzed. Study results and publications are available on the CMAPS website.
There are four main components of CMAPS:
- The Community of Practice: The CoP is for service providers or practitioners currently working in a MAP or for other stakeholders interested in learning more about MAPs or who are interested in starting a MAP in their community. CoP resources and activities include a listserv, webinars, roundtable discussions, and the MAP website hosted by CISUR. There is also an Indigenous-focused CoP running parallel to the main CoP.
- Qualitative interviews: The CMAPS team interviews current and past MAP participants in a number of sites across Canada as well as MAP staff on a range of topics pertaining to program operation and implementation. Areas of investigation include the benefits and challenges of MAP, program rules, protocols and policies and the impact of MAP on various aspects of life. Please contact the CoP Coordinator if you are interested in learning more about the qualitative methods or accessing the CMAPs interview guide.
- Quantitative surveys: The CMAPS team conducts structured quantitative surveys with MAP participants and locally recruited control participants in MAP sites across the country. New MAP participants are followed-up monthly for up to 12 months. The monthly surveys measure:
- Housing quality, stability and satisfaction
- Alcohol consumption and other substance use including non beverage alcohol
- Physical health
- Mental health
- Harms related to alcohol use
- Access to health services
- Quality of life
- Demographic information
- Secondary data: We access secondary administrative data from a variety of sources for both MAP and control participants to see how participating in MAP impacts participants’ service use compared to that of controls. We seek informed consent from all participants to access a range of secondary data including:
- ER visits and hospital admission data
- Alcohol treatment service use
- Liver function test results
- Police contacts
- Corrections data
- MAP administration data, including alcohol administration data
- Death record data
- Shelter use data
Our research protocol has been approved by the University of Victoria Human Research Ethics Board (protocol #13-002) as well as upwards of 30 additional institutional ethics boards across the country. If your community has a MAP or is starting a MAP and you are interested in doing an evaluation please connect with our CoP coordinator to learn more about our research protocols.
About our CoP
The project includes a collaboratively-driven and goal-orientated action-learning community of practice (CoP) component that brings together researchers and knowledge users from across the country to share knowledge and develop expertise around the practice of MAPs. The CoP consists of synchronous learning activities including a virtual seminar series of webinars (see "Resources" tab) involving leaders with direct experience in MAPs and virtual roundtable meetings involving researchers and practitioners. A key function of the CoP is to promote discussion of current evidence as well as protocols and best practices for managed alcohol programs. If you are interested in becoming involved in our CoP, please email Jenny Cartwright. You can also view/subscribe to our e-newsletter and join our listerv.
Researchers
- Dr. Bernie Pauly (PI)
- Dr. Tim Stockwell (PI)
- Dr. Jinhui Zhao
- Sybil Goulet-Stock
- Dierdre Ratenberg
- Brittany Graham (Coordinator)
- Jenny Cartwright (Research Manager)
- There are over 50 additional co-investigators, knowledge users, collaborators, students and community partners working with us on the study.