Nurse researcher points to new pathway for end-of-life care
- Kate Hildebrandt
When Kelli Stajduhar was handed the 2017 Ehor Boyanowsky Academic of the Year Award last month from the Confederation of University Faculty Associations of BC, she was acknowledged as “a living ambassador for the very real difference scientific knowledge brings to revolutionizing health care,” and for “working with nurses on the front lines for more than 30 years to improve point of care services.”
That “point of care” is the end point, better known as palliative care.
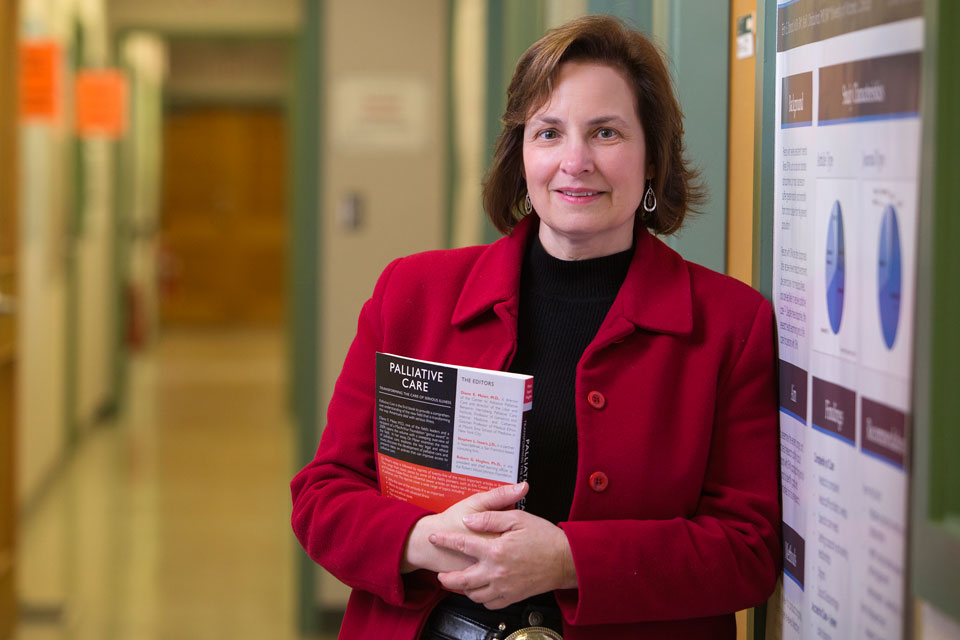
Stajduhar is a professor and co-associate director of research and scholarship with UVic’s School of Nursing, and a lead investigator with UVic’s Institute on Aging and Lifelong Health. Her research work with the Initiative for a Palliative Approach in Nursing: Evidence and Leadership (iPANEL) has convinced her of a way to provide more inclusive, albeit untraditional, palliative care services where nurses take the lead.
That’s what makes her work award-winning. Stajduhar’s findings show what needs to change within our care system so that anyone near death can access the supports they need in a safe and comfortable place, least of which is an acute care hospital ward. “There’s this gap in our understanding about dying and care service delivery,” she says.
“Better care means exploring ways to deliver a palliative approach in any number of settings, not just a hospital or a hospice.” Case in point: homeless Canadians with chronic diseases dying in the streets. After hearing desperate stories from community outreach workers, Stajduhar spoke out.
“We place a high value on palliative care services in Canada, yet we don’t acknowledge its lack of availability,” said Stajduhar in letters to newspapers and at public speaking events. Armed with grace and hard facts, she explained what dying was like for the poorest, most marginalized people in our cities. Her powerful argument yielded a blitz of coverage that placed her on UVic’s top 10 list of newsmakers in 2016.
Stajduhar recalls the story of a homeless man from her study who was in hospital with a terminal illness, later discharged to a local motel. “It was not a great situation,” she explains. “He was living in squalor conditions." All he wanted was to be on the water in a boat where he spent most of his life fishing for a living.
"We could not support that wish for a number of reasons," says Stajduhar. "The sad part was he had no family, just a few friends from the boating community. In his final stage before death, he asked staff from our research team to be with him as he passed."
“Our system is not set up to care for people like this man,” she says, adding that some of us make our home where we can. "Homeless people are no different from anyone else facing death in their desire to stay in their community, wherever that may be, and close to people they know."
While the spotlight and accolades promote understanding, she’ll tell you they’re more a means to an end. “Palliative care needs to be delivered where the patient is at and most comfortable, surrounded by the familiar and cared for by people they know and trust.” For the most part, she says, nurses are already there.
“We just need to figure out the model and policy that will let us do that. For everyone.”

